What is paediatric asthma?
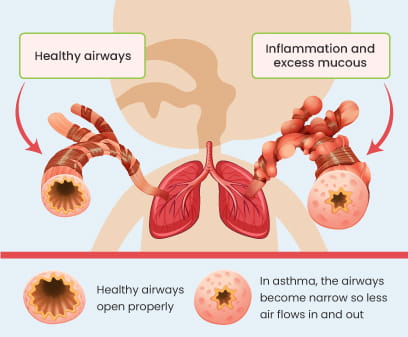
Asthma is a long-term (chronic) condition where your child’s lungs can get irritated by being exposed to various triggers such as cold weather, pollen, etc. When this happens, the inside of the airways swell up, and produce more mucus and the muscles around the airways get tight making it difficult for you to breathe1
Asthma often starts when kids are young, and it's more common in boys than girls.
Fortunately, there are effective treatment options available to manage asthma symptoms and improve their quality of life.
How common is asthma in childhood?
Asthma is a common disease in children. Recent data shows that worldwide,
.svg?updated=20241115085243)
Around 9-10% of Children aged 6-14 worldwide have asthma
.svg?updated=20241115085247)
The total burden of asthma in India is 34.3 million
.svg?updated=20241115085253)
Accounting for 13.09% of the global burden.3
.svg?updated=20241115085258)
The occurrence rate is notably higher among boys and in urban areas.5
.svg?updated=20241115085303)
The number of children affected by this condition is going up over time.4,6,7
Symptoms of paediatric asthma
When kids have asthma, they might experience-:
.svg?updated=20241115085441)
Recurrent coughing.
.svg?updated=20241115085448)
Have ongoing wheezing (a high-pitched whistling sound made while breathing), especially when sleeping or triggered by activities like crying or laughing.
.svg?updated=20241115085454)
Worsening of asthma symptoms at night or early in the morning.
.svg?updated=20241115085500)
Tightness in their chest or trouble breathing, such as feeling out of breath or breathing quickly.
.svg?updated=20241115085505)
Feeling tired from not sleeping well.
.svg?updated=20241115085510)
Act cranky or easily upset.
These symptoms can vary from being not too bad to very severe. Sometimes, worsening symptoms can lead to severe health risks, indicating a worsening of the condition. During this time, symptoms such as increased wheezing, shortness of breath, coughing (especially at night), lethargy, reduced exercise tolerance may occur. If your child shows any of these signs, it is crucial to seek medical help immediately.4
Triggers of paediatric asthma
.svg?updated=20241115085527)
Viral Infections
Pathogenic agents like viruses can cause infections in the lung passages. Viral infections can cause the airways to become inflamed, leading to wheezing and possibly developing into asthma.9
.svg?updated=20241115085532)
Allergens & Irritants
Your child may have allergies to things like dust and pollen grains. Other factors include dust mites, pet dander, etc., which can trigger their symptoms. Certain environmental triggers, like air pollution, gases, strong odours from coils, cooking smells, sprays, or smoke, can irritate your child's airways and worsen their symptoms.
.svg?updated=20241115085537)
Exercise
Physical activities (strenuous play or exercise) can sometimes cause wheezing, coughing, and a feeling of chest tightness in children with respiratory issues due to the narrowing of airways.
.svg?updated=20241115085545)
Stress & Emotions
When your child feels stressed, it can cause shortness of breath and exacerbate their symptoms.1,4,10
Risk factors of childhood asthma
Factors that could raise the likelihood of your child developing asthma include:
.svg?updated=20241115085355)
Viral infections can significantly impact both the development and exacerbation of asthma. If your child gets viral infections a lot, it might increase the chances of them developing asthma.9,18
.svg?updated=20241115085401)
Having previous allergic reactions, i.e., food allergies.
.svg?updated=20241115085406)
A family history of asthma or allergies.
.svg?updated=20241115085411)
Living in areas with a lot of pollution.
.svg?updated=20241115085418)
Being overweight.
.svg?updated=20241115085423)
Having ongoing respiratory issues, such as rhinitis.
.svg?updated=20241115085428)
Maternal obesity and weight gain during pregnancy heighten the likelihood of asthma in offspring.
.svg?updated=20241115085434)
Being around tobacco smoke during pregnancy and childhood raises the risk of developing asthma.4,11,12

.svg?updated=20241115085223)
.svg?updated=20241115085233)
.svg?updated=20241115085228)
.svg?updated=20241115085238)
.svg?updated=20241115085324)
.svg?updated=20241115085328)
.svg?updated=20241115085345)
.svg?updated=20241115085334)
.svg?updated=20241115085340)
.svg?updated=20241115085350)


.svg?updated=20241115085515)
.svg?updated=20241115085520)
.svg?updated=20241115085203)
.svg?updated=20241115085208)
.svg?updated=20241115085213)
.svg?updated=20241115085218)